“20/Unhappy”

Vision beyond 20/20: Unraveling the world of scleral lens HOA correction
“Which is better, one or two?” asks the doctor, to which the patient responds with “Neither.” This encounter may sound familiar to many eye care practitioners, particularly when refracting patients with irregular corneas. Fortunately, scleral lenses have revolutionized vision correction for these patients. The fluid reservoir that rests beneath the scleral lens and above the cornea masks most optical distortions caused by irregularities of the anterior corneal profile, which is particularly helpful in patients with conditions like keratoconus, pellucid marginal degeneration, post-penetrating keratoplasty, and other irregular corneal conditions (1). After a scleral lens is fit appropriately, the lens offers a stable platform for the addition of sphero-cylindrical optics. Despite these characteristics, patients wearing scleral lenses may still be “20/Unhappy”, and aberrations are likely to blame. Fortunately, technology advancements allow for the accessibility of state-of-the-art optical correction with higher-order aberration (HOA) correction in scleral lenses.
Understanding Aberrations
In a perfect optical system, light will refract to a precise point; however, even in eyes with seemingly “perfect”, emmetropic vision, there is some variation from this precise point. These variations are defined as aberrations (2,3).
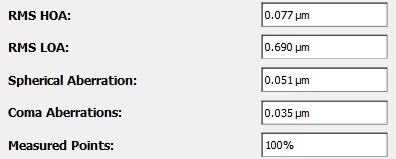
In order to quantify these deviations, aberrations can be broken down by type and severity through Zernicke polynomials and Root mean square calculations (RMS). Each Zernike polynomial describes a specific aberration, like astigmatism or spherical aberration (4). Root mean square (RMS) is a mathematical measure used to quantify the overall magnitude of these aberrations, calculated from the coefficients of the Zernike polynomials (4). The RMS value is typically expressed in micrometers (µm) and helps the practitioner to better understand the optical quality of the eye. A lower RMS value indicates fewer aberrations and better optical quality, while a higher RMS value suggests more aberrations and potentially poorer vision quality (see figure 1).
Aberrations of the eye can be broadly categorized into two groups – lower order aberrations and higher order aberrations.
Lower order aberrations (LOA): LOAs such as defocus and astigmatism are correctable with traditional glasses and contact lenses through sphero-cylindrical correction. Typically, in patients without corneal disease, sphero-cylindrical correction is sufficient in providing clear and precise vision (5).
Higher order aberrations (HOAs): HOAs are optical imperfections that extend beyond lower order aberrations. Clinically applicable HOAs include coma, trefoil, and spherical aberration. HOAs are characterized by complex wavefront distortions that result from variations in the shape of the cornea, lens, and other optical components of the eye. Symptoms of HOAs include reduced contrast sensitivity, glare and haloes, difficulty with night vision, visual distortion, and/or reduced visual acuity despite optimal sphero-cylindrical correction (5).
Necessary Steps Before Addressing HOAs
Start with Full LOA correction: Before addressing HOAs, it is essential to ensure that the patient’s vision is optimally corrected in the scleral contact lens. Achieving accurate and stable spherico-cylindrical corrections forms the foundation for managing HOAs.
Avoid inducing HOAs: Due to the shape of the sclera, scleral lenses typically decenter inferior-temporal (7). Decentration of scleral lens optics can induce or exacerbate HOAs, particularly coma (6). Customizing the edge profiles (haptics) of scleral lenses and ensuring proper central and limbal tear clearance can help optimize the centration of scleral lenses (8).
Quantifying HOAs
Patient feedback: Subjective feedback from patients can provide insight on the visual impacts of HOAs (9). Do the letters seem to be smeared on the chart? Are you seeing shadows? At night, do you experience haloes or glare? In some instances, it may be helpful for patients to demonstrate their vision experience through illustrations or drawings.
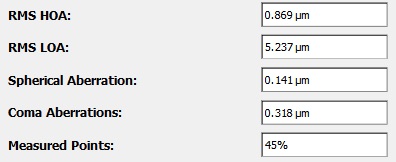
Aberrometer: Aberrometers are instruments that analyze the wavefront of light as it passes through the eye. By measuring the wavefront distortions, an aberrometer can provide a detailed map of both LOAs and HOAs present in the patient’s visual system. This data is valuable for creating custom HOA correction in scleral lenses (10).
Incorporating HOAs into a Scleral Lens
There are several approaches to correcting HOAs in patients wearing scleral lenses:
Front surface eccentricity (FSE): FSE refers to altering the anterior curvature of the scleral lens to compensate for HOAs. FSE helps reduce common aberrations, such as coma and spherical aberrations, the HOA most commonly observed in patients with keratoconus (11,12). A great advantage of utilizing FSE technology is accessibility, such as BostonSight Scleral’s SmartSight FSE. Practitioners utilize the scleral lens fit set which has varying levels of eccentricity, over-refract over the selected lens, and then assess the patient’s subjective vision experience with the over-refraction (see figure 2c).
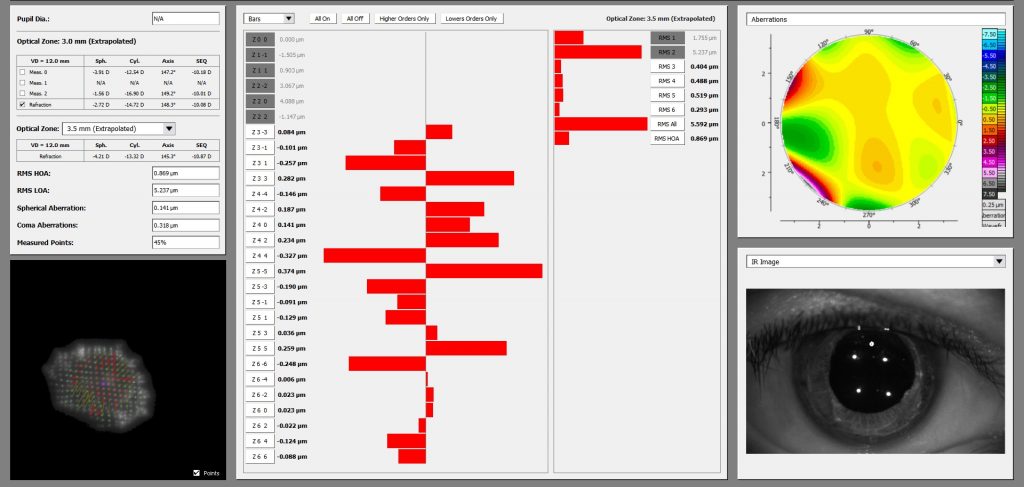
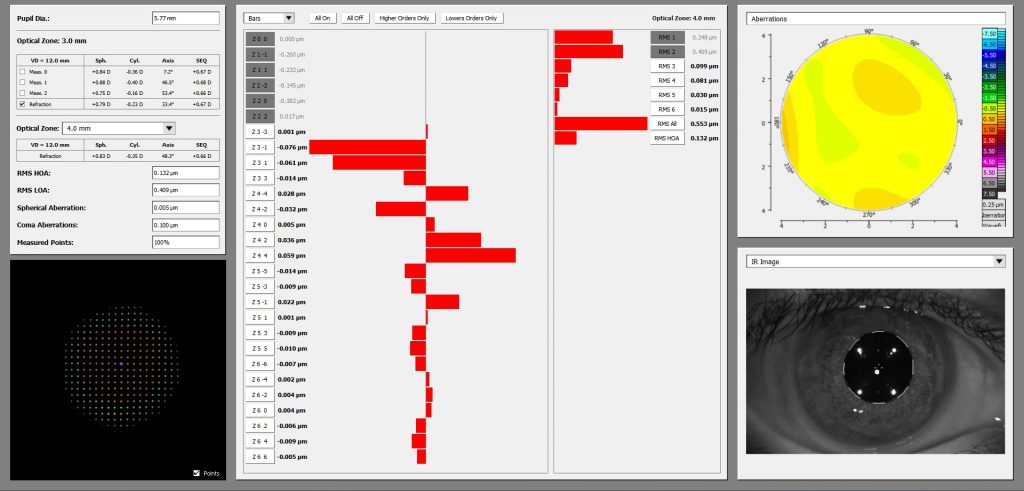
Custom HOA correction: In advanced scleral lens designs, aberrometry data can be utilized and translated into custom HOA optics. This method requires a precise fitting process of the scleral lens to ensure stabilization and centration. Following a proper fit, a lens with markings may be dispensed, and aberrometry is performed to assess for residual HOAs with lens wear. These HOAs can then be added into the scleral lens to provide the patient with the most customized vision solution (13).
Scleral lenses have transformed the lives of individuals with irregular corneas. Now with the accessibility of HOA correction, patients’ troublesome symptoms related to HOAs can be improved with FSE technology or neutralized with custom HOA correction. By embracing this technology, the journey from “20/Unhappy” to “20/Happy” is now within reach.
References
Scleral contact lenses and vision correction for irregular corneas:
1. Brown, A., & Johnson, L. (2020). “Scleral Contact Lenses for Irregular Corneas.” Eye Care Journal, 55(3), 211-225.
2. Johnson, M., & Davis, R. (2018). “Optical Aberrations in Emmetropic Eyes.” Optics and Vision Journal, 32(4), 421-435.
3. Thibos LN, Hong X, Bradley A, Cheng X. Statistical variation of aberration structure and image quality in a normal population of healthy eyes. Journal of the Optical Society of America A. 2002;19(12):2329-2348.
4. Williams, P., & Wilson, S. (2017). “Quantifying Aberrations Using RMS and Zernike Polynomials.” Optics Express, 25(8), 789-802.
5. Anderson, K., & White, L. (2019). “Higher Order Aberrations in Clinical Practice.” Ophthalmic Practice Journal, 41(6), 545-561.
6. Kowalski, Louise P., Michael J. Collins, and Stephen J. Vincent. “Scleral lens centration: The influence of centre thickness, scleral topography, and apical clearance.” Contact Lens and Anterior Eye 43.6 (2020): 562-567.
7. Hall, L. A., Hunt, C., Young, G., & Wolffsohn, J. (2013). Factors affecting corneoscleral topography. Investigative ophthalmology & visual science, 54(5), 3691-3701.
8. Barnett, M., Carrasquillo, K. G., & Schornack, M. M. (2020). Clinical outcomes of scleral lens fitting with a data-driven, quadrant-specific design: Multicenter review. Optometry and Vision Science, 97(9), 761-765.
9. Miller, S., & Jackson, R. (2020). “Patient Feedback in Evaluating HOAs.” Clinical Optometry Journal, 12(3), 213-225.
10. Roberts, M., & Smith, D. (2019). “Aberrometry and Its Applications in Vision Correction.” Journal of Optometric Technology, 48(2), 112-128.
11. Taylor, R., & Hall, A. (2018). “Front Surface Eccentricity for HOA Correction in Scleral Lenses.” Contact Lens Research Journal, 37(4), 321-335.
12. Hussoin, T., Le, H. G., Carrasquillo, K. G., Johns, L., Rosenthal, P., & Jacobs, D. S. (2012). The effect of optic asphericity on visual rehabilitation of corneal ectasia with a prosthetic device. Eye & Contact Lens, 38(5), 300-305.
13. Garcia, M., & Martinez, E. (2021). “Custom HOA Correction in Advanced Scleral Lenses.” Optometric Science Journal, 58(7), 621-635.

Dr. Ariel Cerenzie
Dr. Ariel Cerenzie started the Charlotte Contact Lens Institute to focus on specialty lens care after witnessing the profound impact specialty contact lenses have on improving the current and future lives of patients. She is a fellow of the American Academy of Optometry and the Scleral Lens Education Society and is a member of the American Academy of Orthokeratology and Myopia Control.